Pick a Topic:
Find info on a:

ClotCare complies with the HONcode standard for trustworthy health
information:
verify here.
 ClotCare is a member organization of the Coalition to Prevent Deep Vein Thrombosis. Click here to learn more about the Coalition to Prevent Deep Vein Thrombosis and DVT Awareness Month, which is held each March.
ClotCare is a member organization of the Coalition to Prevent Deep Vein Thrombosis. Click here to learn more about the Coalition to Prevent Deep Vein Thrombosis and DVT Awareness Month, which is held each March.
|
Can better INR control be achieved, and if so, how will new anticoagulants compare to warfarin (Coumadin)?
Henry I. Bussey, Pharm.D., FCCP, FAHA
March, 2007
Reference: White HD, Gruber M, Feyzi J, et. al. Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V. Arch Intern Med. 2007 Feb 12;167(3):239-45.
This article is one of several key studies* that are raising important questions about the future role of warfarin therapy, especially in patients with atrial fibrillation.
Is the expanded use of warfarin causing more harm than good, and should we reduce our use of anticoagulation in atrial fibrillation?
Should we be using warfarin to treat more, rather than fewer, patients with atrial fibrillation?
Does improving INR control beyond that typically reported in clinical trials yield an improved risk/benefit ratio? If so, what can be done to improve INR control further? If we can optimize INR control, will there be a need for newer anticoagulants currently in development?
What is the adherence rate of warfarin patients managed in an anticoagulation clinic, and are there clinical consequences of non-adherence in such patients?
This report by White et. al. showed that unusually good control of the INR was associated with a substantial reduction in events in a large population of warfarin-treated patients. White and colleagues performed a sub-group analysis on the pooled data from the SPORTIF III and SPORTIF IV trials (two large prospective trials that compared warfarin to ximelagatran in patients with atrial fibrillation). In these two trials, ximelagatran-treated patients had a major end point event rate of 1.6% for stroke plus systemic embolic event (SEE). The warfarin-treated patients had event rates of 2.3% in one trial and 1.2% in the other trial (both were not significantly different from the event rate in the ximelagatran-treated patients). Overall, ximelagatran was non-inferior to warfarin in terms of efficacy, and major bleeding rates were not significantly different. White and colleagues, however, grouped patients into three groups based on the degree of INR control. Those with the highest percent of in-range INR values (mean time in range of 83%) had approximately a 50% lower event rate that did those patients with the lowest in-range values (mean in range time of 48%). (see table 1 below) The event rates are so much lower in the well-controlled warfarin patients that it raises two more questions:
-
Can we find ways to achieve this level of anticoagulation control in all patients?
-
If such optimal control of the INR can be reasonably achieved, is it feasible to anticipate that any of the agents in development will be able to compete with warfarin in terms of safety and efficacy?
Table 1. Event rates based on INR control & ximelagatran treatment
|
|
Poor
(< 60%)
48%
n = 1190
|
Mod.
(60 - 75%)
68%
n = 1207
|
Good
(> 75%)
83%
n = 1190
|
Ximelag.
|
|
Stroke + SEE
|
2.1
|
1.34*
|
1.07**
|
1.6**
|
|
Maj. Bleed
|
3.85
|
1.96***
|
1.58**
|
no diff**
|
|
Mortality
|
4.2
|
1.84***
|
1.69**
|
|
M. I.
|
1.38
|
0.89
|
0.62**
|
|
Total
|
11.53
|
6.03
|
4.96
|
*trend mod. vs poor
**stat. diff good vs poor, none was stat. diff good vs mod.
***stat. diff mod vs. poor
White HD, et al. Arch Intern Med. 2007; 167:239-245.
One study suggests that better patient education might reduce complication rates presumably by achieving better INR control. In a study of elderly patients on warfarin, those who rated their patient education as insufficient were found to have a major bleeding rate of almost 9 times that seen in patients who considered their patient education to be good.1
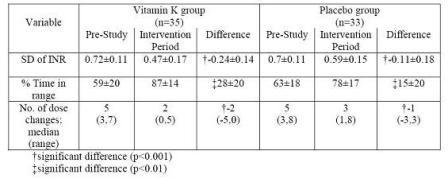
Further, Veeger and colleagues recently pointed out that one-fourth of warfarin treated patients with the poorest INR control had INRs in range only 10% to 20% of the time, yet these patients accounted for most of the adverse events.2 Others have reported that, with the addition of a small daily dose of vitamin K, poorly controlled patients can double their in-range INR values 3 (see table 2) and that patients with relatively good INR control can achieve substantially better INR control4 (see table 3).
Table 2. INR control before & after vit. K supplementation
|
|
% INRs in range
|
% INRs in range + 0.2
|
|
Patient
|
Before
|
After
|
Before
|
After
|
|
1
|
54
|
60
|
69
|
77
|
|
2
|
0
|
41
|
33
|
55
|
|
3
|
7
|
53
|
36
|
76
|
|
4
|
9
|
18
|
17
|
47
|
|
5
|
8
|
38
|
33
|
46
|
|
6*
|
37
|
36
|
37
|
36
|
|
7
|
0
|
100
|
0
|
100
|
|
8
|
27
|
30
|
45
|
38
|
|
Group
|
18*
|
42*
|
32
|
57*
|
*Patient 6 was later found to have lupus anticoagulant (which can falsely elevate the INR) and a hyperfunctioning thyroid nodule (which can cause wide fluctuations in the response to warfarin).
Reese AM, et al. Pharmacotherapy 2005; 25:1746-1751.
Table 3. INR control before & after vit. K supplementation
Blood. 2007 Mar 15;109(6):2419-23. Epub 2006 Nov 16.
In addition to daily vitamin K supplementation, others have suggested that patient self-testing and self-management also may improve INR control (see table 3). However, in my opinion, the degree of INR control in these reports did not achieve what might be considered optimal INR control. If one-third of more than 3,500 patients in the SPORTIF trials achieved in range INRs 83% of the time, might there be a way to achieve similar INR control in all patients? I believe that combining daily low dose vitamin K with frequent self-testing and online computer assisted management can achieve this goal while making anticoagulation management more convenient and less costly for both clinicians and patients. Do I have data to support that contention? Not yet.
Table 4. INR control and major adverse event rates with self-management (SM) vs. anticoagulation clinic management (AC)
|
|
Italian Studya
n=368 v 369
|
UK Studyb
N=337 v 288
|
Maj. A.E. - AC gp
- SM gp
|
7.3
2.2
|
2.7
2.8
|
|
In Range - AC gp
- SM gp
|
56
59
|
68
70
|
2.5 target gp - AC
- SM
|
|
71
74
|
3.5 target gp - AC
- SM
|
|
53
55
|
|
SM gp Dropout
|
|
21%
28%
|
a. Menendez-Jandula, et al. Ann Intern Med 2005; 142:1-10.
b. Fitzmaurice, et al. BMJ 2005 (Oct. 10):1-6.
Additional Questions About Warfarin's Future
-
Should we be treating fewer patients with warfarin (Coumadin)?
-
Should we be treating more patients with warfarin (Coumadin)?
Additional References
-
Kagansky N, Knobler H, Rimon E, Ozer Z, Levy S. Safety of anticoagulation therapy in well-informed older patients. Arch Intern Med. 2004 Oct 11;164(18):2044-50.
-
Veeger NJ, Piersma-Wichers M, Hillege HL, Crijns HJ, van der Meer J. Early detection of patients with a poor response to vitamin K antagonists: the clinical impact of individual time within target range in patients with heart disease. J Thromb Haemost. 2006 Jul;4(7):1625-7.
-
Reese AM, Farnett LE, Lyons RM, Patel B, Morgan L, Bussey HI. Low-dose vitamin K to augment anticoagulation control. Pharmacotherapy. 2005 Dec;25(12):1746-51.
-
Sconce E, Avery P, Wynne H, Kamali F. Vitamin K supplementation can improve stability of anticoagulation for patients with unexplained variability in response to warfarin. Blood. 2007 Mar 15;109(6):2419-23. Epub 2006 Nov 16.
|
ClotCare is a 501(c)(3) non-profit organization generously supported by your tax-deductible donations and grants from our industry supporters.
New Postings:
Click here to view full list of new postings
|