Understanding Deep Vein Thrombosis
(DVT = Blood Clot, Usually in the Leg)
DVT & PE Risks, Symptoms, Diagnosis, Prevention, & Treatment
Stuart T. Haines, Pharm.D., BCPS
March 2004
Updated May, 2006 by Henry I. Bussey, Pharm.D. & Jan., 2007 by Marie B. Walker
Deep Vein Thrombosis
A deep vein thrombosis (DVT) is a potentially deadly condition caused by a blood clot that forms in a vein - most commonly the deep veins in the legs. This clot formation can happen if the vein is damaged or if the blood flow in the vein is slow or stops. DVT can cause pain and swelling in the leg, but many times it produces no symptoms. If the clot breaks off and travels in the bloodstream, it can cause damage to the lungs. When a blood clot travels to the lungs, it is called a pulmonary embolism (PE). A PE often causes shortness of breath and chest pain. If the lung damage is severe, it can kill people very quickly, even before treatment can be given. For this reason, every effort should be made to prevent a DVT before it happens. Although there are several effective methods to prevent blood clots, a recent study found that more than one-half of patients who developed a DVT in the hospital did not receive any of these preventive methods. For more information on this study, go to the DVT Prophylaxis page of our site.
Although you may have never heard about it before, DVT is a common medical problem. It is estimated that 2 million people in the United States develop a DVT every year -- many of them don't even know it. Of those who develop a pulmonary embolism, up to 200,000 die each year, which is more than die annually in the US from breast cancer and AIDS combined.
Who gets a DVT?
Some people are more prone to getting blood clots in the leg. The chances of getting a DVT increase as we age and doubles with each decade of life over the age of 40. For example, someone who is 80 years old is twice as likely to get a DVT as someone who is 70 years old and 16 times more likely than someone who is 40 years old. People who have had a DVT in the past are at a much higher risk of getting another DVT. Additionally, some people inherit conditions from their parents that make them more prone to forming blood clots.
Other factors that increase the risk of getting a DVT include:
-
major surgery under general anesthesia, especially if it involves leg joints or a hip
-
obesity
-
varicose veins
-
prolonged bed rest and immobility
-
heart or lung problems that require hospitalization
-
major injuries
-
cancer
-
leg paralysis
-
pregnancy and childbirth
-
estrogen containing contraceptive pills, patch, or vaginal ring
-
estrogen replacement therapy
-
long-distance travel
Symptoms of a DVT
When a blood clot forms, it can either partially or totally block the flow of blood in the vein. Smaller blood clots that partially block blood flow may cause only mild symptoms or none at all. Larger blood clots that block blood flow usually cause:
-
leg swelling
-
leg pain -- often worse when standing or walking
-
leg warmth and redness
Problems caused by a DVT
A small blood clot below the knee is unlikely to cause symptoms or complications. However, if a clot extends or forms above the knee, it may break away, travel in the blood, and block a blood vessel in the lung. A clot that blocks a blood vessel in the lung is called a pulmonary embolism (PE). People who get a PE may develop sudden shortness of breath, coughing, or chest pain. Depending on the size of the clot, a PE can be life-threatening.
DVTs frequently damage the valves in the leg veins. Valves in the leg veins help blood to flow upward toward the heart and prevent blood from flowing backward toward the feet. When these valves become damaged by DVT, the blood pools in the leg instead of flowing upwards toward the heart. This pooling of blood can cause chronic leg swelling and pain, as well as skin changes and leg sores. This condition is called the post-thrombotic syndrome. The pain from post-thrombotic syndrome often remains even after you have stopped taking warfarin and/or after a clot has dissolved. Click here to learn more about post-thrombotic syndrome.
Diagnosing a DVT
If a DVT is suspected, a physician must order tests to determine if a blood clot is present in the leg. The most common tests used to determine if there is a DVT are:
-
a d-Dimer test (to learn more about the d-Dimer test, click here)
-
an ultrasound scan of the legs - This test is very good for identifying large clots above the knee in patients who have symptoms, but it may not be that good in identifying small clots below the knee in patients who have little or no symptoms.
-
blood samples to check for clotting problems (such as inherited biochemical conditions that may increase one's risk of developing a DVT)
-
a venogram - This test is the "gold standard" for confirming a clot inside a vein, but it involves injecting a dye into the veins in the foot and then taking an x-ray of the veins in the leg to see if there is a clot present. The dye may cause some discomfort when injected and, in some cases, may even stimulate the blood to clot. Consequently, venograms are usually reserved for clinical studies and/or when the ultrasound result is uncertain.
Preventing a DVT
By far the best approach is to prevent a DVT before it happens. People who have one or more risk factors for a DVT should learn about ways to prevent it. You should know your risk for DVT. Click here to get a copy of the DVT Coalition's DVT risk assessment tool. There are few things that anybody can do to help prevent a DVT including:

-
exercising the legs regularly -- take a brisk walk every day
-
maintaining a reasonable body weight
-
avoiding sitting or lying in bed for long periods of time
-
avoiding tight-fitting, restrictive clothing
-
sitting with both legs on the floor (uncrossed)
People who are hospitalized are at higher risk for developing a DVT. Surgery, especially surgery that involves a leg joint or hip, dramatically increases the risk of having a DVT. Therefore, at the time of admission to a hospital, a health care practitioner should do a careful DVT risk assessment. Various methods can be used to keep the risk of DVT as low as possible. This may include anticoagulant medicines that inhibit the blood's tendency to clot. Anticoagulant medicines are often referred to as "blood thinners," but they do not actually thin the blood. Rather, they reduce the body's ability to form a blood clot. In some cases, an intermittent compression device that automatically squeezes the feet and lower legs is used to increase the blood flow in the legs.
Although the risk of developing a DVT during long-distance travel is quite low, it is a good idea to exercise the legs at least once every hour during the trip. Regular exercise at least once every hour means taking regular breaks if driving or walking the aisle if traveling by train, bus, or airplane. Travelers who are at risk of developing a DVT may wish to wear graduated compression stockings. These compression stockings can be purchased in different lengths and are designed to provide different levels of compression pressure. A patient should consult his/her healthcare provider for advice on which design and pressure gradient would be best for him or her. Click here to learn more about graduated compression stockings, including information on where to get them.
People who have had a DVT in the past or have multiple DVT risk factors should seek medical advice before traveling long-distance. Some doctors recommend taking a dose of aspirin or anticoagulant medicine before traveling. But this approach is not suitable for everyone, and there are potential side-effects.
Anyone who suddenly develops leg pain and swelling or breathing problems within a week after being in a hospital or taking a long-distance trip should immediately seek medical advice.
Treating a DVT
Once a DVT is suspected and diagnosed, prompt treatment is required. The purpose of treatment is to prevent:
-
the clot from getting bigger
-
the clot from traveling to the lungs
-
new clots from forming
-
the post-thrombotic syndrome
The most common treatment for a DVT is anticoagulant medicines. Anticoagulants such as heparin or low molecular weight heparin (LMWH) are initially given in an arm vein or injected just under the skin for several days. Common brand names of these drugs include Lovenox, Innohep, Fragmin, and Arixtra. The purpose of these anticoagulant medicines is to turn off the clotting system in the body.
After a few days, most patients begin taking warfarin (brand name Coumadin) tablets by mouth. The heparin or low molecular weight heparin is continued with the warfarin for at least 5 days. The heparin or low molecular weight heparin should not be stopped until the patient's INR is in range and stable. The INR is the test used to measure the effectiveness of warfarin. Anticoagulation drugs require regular blood tests (the PT-INR test) to check if too little or too much of the drug is being taken. Click here to learn more about the INR.
Warfarin works differently than heparin and low molecular weight heparin. Whereas heparin/LMWH work to turn off the clotting system, warfarin works to keep the clotting system from becoming activated once it has been turned off. The length of time that a patient will need to take warfarin depends on what caused the blood clot and if the patient has had blood clots in the past. If it's the patient’s first blood clot and it was provoked by a temporary cause, such as trauma or surgery, then 3 months of anticoagulation may be enough. If the clot was unprovoked or caused by a chronic condition, the usual recommendation is to treat with anticoagulation for at least 6 to 12 months. If the patient has had two or more unprovoked recurrent clots or if there is a biochemical condition that increases the risk of clot formation, then warfarin may be continued life-long. There are some clinicians who favor life-long anticoagulation after a single unprovoked DVT or PE.
Anticoagulants can't dissolve clots, but they can stop new blood clots from forming and existing ones from growing. The body will often dissolve the clot over time. Click here to learn more about the possibility of a clot remaining in your body indefinitely.
Clot "busting" drugs called thrombolytics are sometimes used to dissolve a DVT. These medicines must be used soon after the clot develops and can cause very serious bleeding problems, so they are only used in severe cases where life or limb is threatened.
To reduce the swelling caused by DVTs and to prevent post-thrombotic syndrome, some doctors recommend wearing graduated compression stockings. These stockings should be worn throughout the day, can be purchased in different lengths, and are designed to provide different levels of compression pressure. A patient should consult his/her healthcare provider for advice on which design and pressure gradient would be best for him or her. Click here to learn more about graduated compression stockings.
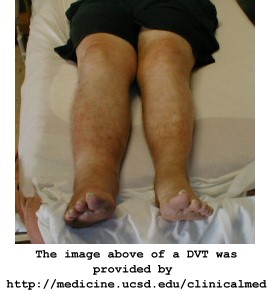
What does a DVT look like?
Below are a few images of deep vein thrombosis. All images are courtesy of Charlie Goldberg, M.D. and Jan Thompson, whose website is located at http://medicine.ucsd.edu/clinicalmed.
Further information
The following resources have additional information on deep vein thrombosis:
Circulation Patient Pages
The journal Circulation has a section known as "Patient Pages." Below are links to 3 "Patient Page" articles dealing with deep vein thrombosis and pulmonary embolism.
Goldhaber SZ, Morrison RB. Pulmonary Embolism and Deep Vein Thrombosis. Circulation. 2002;106:1436-1438.
Goldhaber SZ, Grasso-Correnti N. Treatment of Blood Clots. Circulation. 2002;106:e138-140.
Goldhaber, SZ, Fanikos, J. Prevention of Deep Vein Thrombosis and Pulmonary Embolism. Circulation. 2004:110e445-e447.
National Library of Medicine MedlinePlus Website
http://www.nlm.nih.gov/medlineplus/thrombophlebitis.html.
DVT.net
DVT.net is a resource provided by sanofi-aventis, US, L.L.C. that provides information on deep vein thrombosis. The information provided on this site is intended for patients and caregivers. The site offers animations that explain deep vein thrombosis, unstable angina, the clotting mechanism, and the cardiovascular system.
http://www.dvt.net
U.S. Website for Lovenox
The U.S. Website for Lovenox is provided by Aventis, the maker of Lovenox. This site has information for healthcare professionals and for patients/caregivers.
http://www.lovenox.com
Coalition to Prevent Deep-Vein Thrombosis
The Coalition to Prevent DVT serves "to reduce the immediate and long-term dangers of deep-vein thrombosis (DVT) and pulmonary embolism (PE), which together comprise one of the nation's leading causes of death. The Coalition will educate the public, healthcare professionals and policy-makers about risk factors, symptoms and signs associated with DVT, as well as identify evidence-based measures to prevent morbidity and mortality from DVT and PE." (Mission statement as it appears on www.preventdvt.org)
http://www.preventdvt.org
|